Ensuring safe and effective treatment of bone defects is the top priority for clinicians. However, treating musculoskeletal disorders is increasingly complex due to the diverse characteristics of patients. Aging and diseases such as osteoporosis may impair bone regeneration, while young patients and children exhibit significantly accelerated healing progress. Advancements in technology and data accessibility offer promising solutions for the daily challenges in orthopedic and trauma care.
Setting up digital twins for clinical insights
OSORA develops and builds patient-specific digital twins that can be utilized to evaluate bone defects. Here is what it takes to build a setting that generates meaningful results:
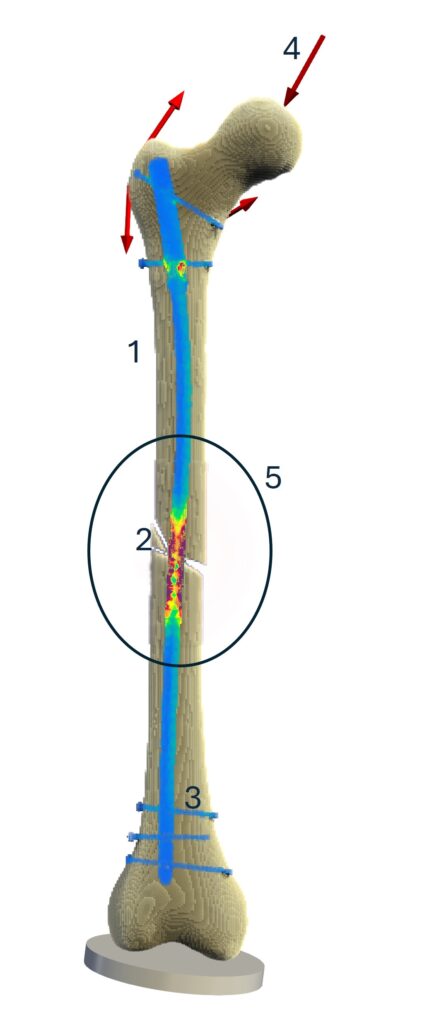
1. Bone Structure (Yellow)
Representing the shape and size of the bony structure, the 3D geometry forms the basis of the digital twin. The reconstruction can be achieved through various medical imaging modalities such as CT scans or biplanar X-rays, complemented by statistical information on the bone. Bone quality, such as in osteoporotic conditions or other illnesses, influences bone density and material parameters, with lower density bones being significantly weaker than healthy ones.
2. Defect/Fracture Topography
Bones provide stability to our body. When they break or osteotomies are required, fractures of varying complexity occur. These defects can heal naturally if mechanical and biological conditions are conducive to new bone formation.
3. Implant Configuration (Blue, FEM)
Surgeons achieve mechanical stability of the bone through conservative or operative treatments. In a digital twin, various implant configurations can be tested before being applied to the patient. Different types of implants, lengths, and screw configurations can be evaluated. By using numerical methods like the Finite-Element-Method (FEM), the stability of an implant can be assessed throughout the healing process. As visualized in the animation, the load on the implant (shown in red) decreases over time as the healing bone takes over the load.
4. Loading on the Bone (Red Arrows)
Bone regeneration takes several weeks, during which patients should still be able to move. Depending on the body part and the osteosynthesis design, different weight-bearing scenarios are possible for the rehabilitation regime. For example, the femur can be subjected to muscle and joint forces during walking (Heller et al.). Applying partial or full weight-bearing influences has effects on bone healing and is a crucial part of patients’ compliance during rehabilitation.
5. Fracture Healing (Circle)
If the balancing of factors is favorable, the tissue in the fractured area evolves into bone again (Giannoudis et al.). Under optimal conditions, cartilage (blue) and woven bone (orange) form a soft callus that matures into calcified stable bone. This process is included in the digital twin through a dynamic tissue-level simulation model (Engelhardt et al., Niemeyer et al.). Each patient’s healing process is influenced by various factors, including concomitant diseases and biological conditions, which alter therapy requirements. To account for these phenomena and evaluate the entire patient, OSORA develops an AI-powered simulation orthopedic planning approach.
Benefits of Digital Twins in Clinical Decision-Making
Our digital twin technology forms the foundation for simulation and AI-supported clinical decision-making. Early monitoring of fracture healing is crucial for identifying the healing potential. However, in the initial weeks post-hospitalization, monitoring is limited to subjective assessment and functional monitoring. The first invasive X-ray check often does not produce enough information on bone formation. By visualizing the healing process via digital twins, both patients and clinicians can understand the patient-specific healing pattern. Surgeons can use the predicted bone formation to assess if the bone will heal, or if changes to the therapy approach may be necessary.
By understanding which therapy approaches are favorable, we can improve the entire treatment process for patients and physicians, but also enhance implant performance through continuous improvement. This comprehensive approach not only will create benefits for improved patient outcomes, but also advances the field of orthopedic surgery as a whole.
