Take aways from the case discussion in the trauma course
Fundamental prinicples
Primary vs. secondary healing
Direct bone formation
-
Requires direct bone contact or small gaps and does only tolerate small interfragmentary movement → absolute stability
-
This can be achieved surgically only by open anatomical reduction and absolutely stable internal fixation with interfragmentary compression or a small stable gap.
-
Strain theory of Perren and Cordey: direct bone formation can only occur if the interfragmentary strain is smaller than the failure strain of the newly formed bone tissue [1]. Accordingly, only strains less than 2% can allow direct fracture healing [2].
Indirect bone formation
-
A majority of fractures heal via the indirect or secondary route.
-
Secondary fracture healing occurs with relative stability in the fracture area.
-
Relative stability is achieved surgically by indirect reduction and bridging internal (angular stable plate osteosynthesis, intramedullary nailing) or external fixation (external fixator) [3, 4].
-
Even with relative stability, the right amount of interfragmentary strain must be present to achieve successful fracture healing. If the fixation is too rigid or too flexible, delayed healing or non-union will result [5].
References
-
Perren and Cordey. Tissue differences in fracture healing. Unfallheilkunde 80, 161-164 (1977).
-
Perren. Fracture healing: fracture healing understood as the result of a fascinating cascade of physical and biological interactions. Part II. Acta Chir Orthop Traumatol Cech 82, 13-21 (2015).
-
Augat and von Rüden. Evolution of fracture treatment with bone plates. Injury 49, S2-S7 (2018).
-
Hierholzer et al. Entwicklung und Prinzipien der Verriegelungsmarknagelung. Unfallchirurg 121, 239-255 (2018).
-
Lutz Claes. Mechanobiology of fracture healing: From basic science to clinical application. Springer Cham (2022). ISBN: 978-3-030-94081-2
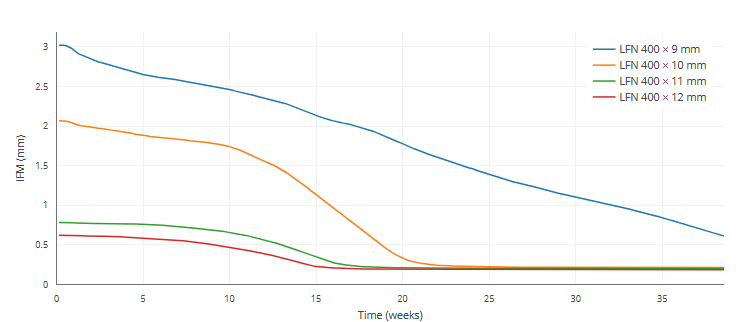
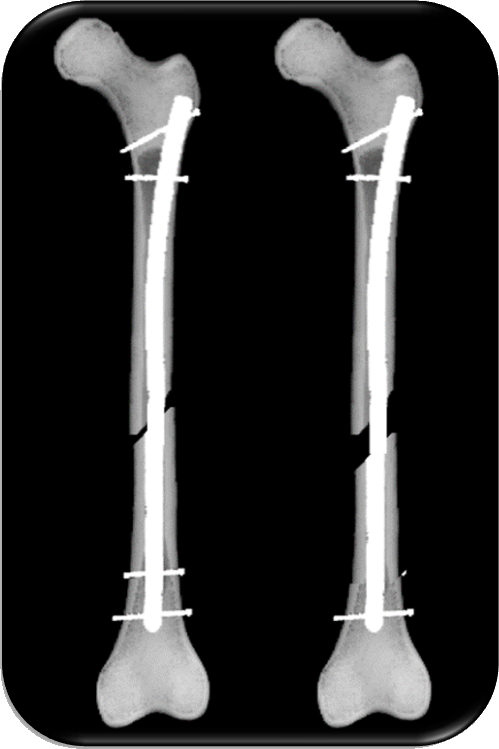
Femur shaft fracture - influence of nail thickness

-
Minimizing shear and torsional movements at the gap promotes fracture healing.
-
Even a slightly bigger nail diameter results in disproportionately increased stiffness.
-
Greater system stiffness, in turn, results in less movement at the fracture gap.
-
The play of the nail inside the medullary cavity should be kept as small as possible.
-
Thus, choosing the largest possible nail diameter makes biomechanical sense, due to its superior stiffness.
References
-
Penzkofer et al. Influence of intramedullary nail diameter and locking mode on the stability of tibial shaft fracture fixation. Arch Orthop Trauma Surg 129, 525-531 (2009).
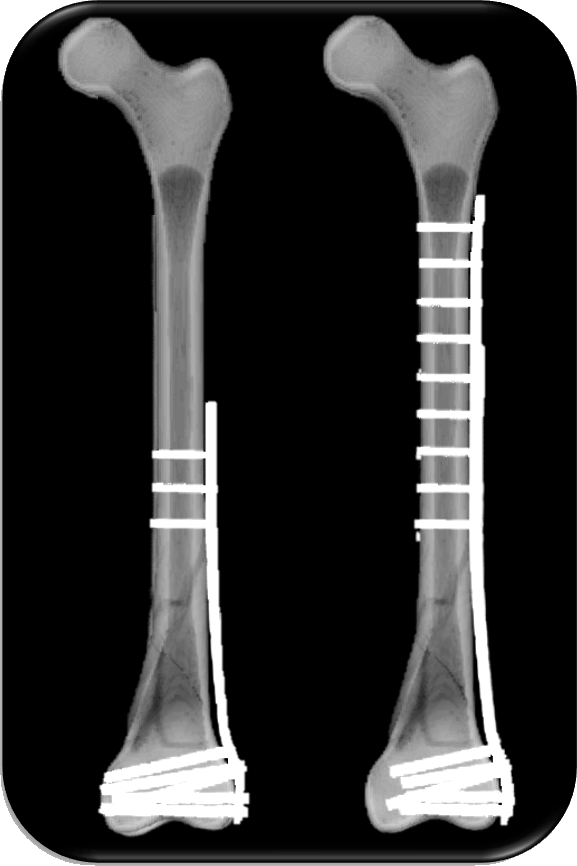
Distal femur shaft fracture
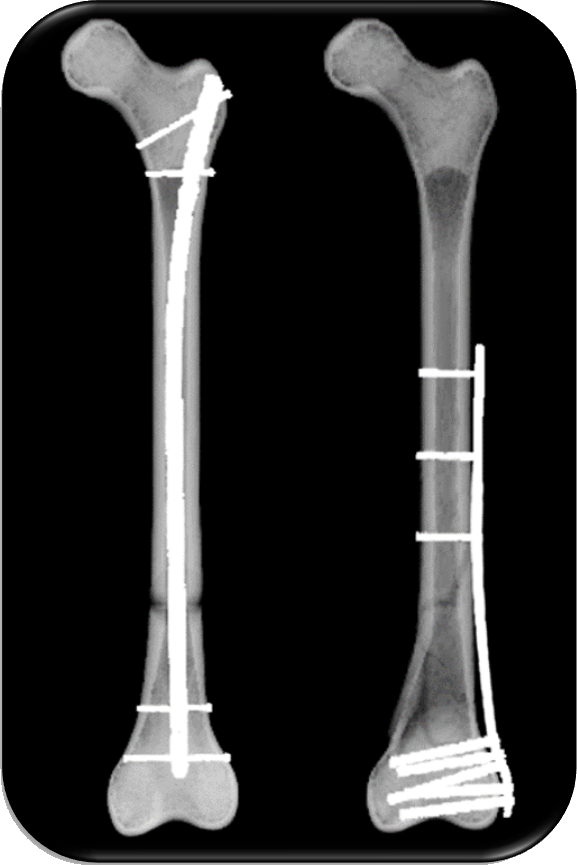
-
Both nail and and plating systems have become reliable treatment modalities for distal femur fractures. [1]
-
While proponents of each treatment modality will debate on pros and cons of both IMN and LP, there is still no clear consensus on a gold standard.
-
Stabilization of distal femur fractures with locking plates can cause inconsistent and asymmetric formation of periosteal callus, which may be attributed to the high stiffness of the fixation construct. [2]
-
Fractures treated with intramedullary nailing were found to have a 93.9% union rate, an average time to union of 19.2 weeks, an average arc of motion of 105.1 degrees, with an average of 14.4 degrees of malalignment. [1]
-
Fractures treated with locking plates were found to have a 90.2% union rate, an average time to union of 20.5 weeks, an average arc of motion of 104 degrees, with an average of 12.6 degrees of malalignment. [1]
References
-
Jankowski et al. Comparing Intramedullary Nailing Versus Locked Plating in the Treatment of Native Distal Femur Fractures: Is One Superior to the Other?. JOIO 55, 646-654 (2021).
-
Lujan et al. >Locked plating of distal femur fractures leads to inconsistent and asymmetric callus formation. J Orthop Trauma 24, 156-162 (2010).
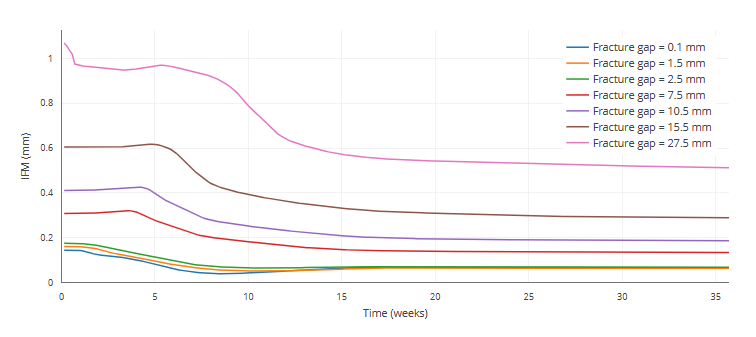
Differences in shaft fractures - influence of fracture gap size
-
The quality of the fracture healing outcome and the rate of healing decreases with increasing fracture gap size.
-
Large fracture gaps can create critical size defects that supress healing and lead to non-unons.
-
A critical size defect might be defined as exceeding 1.5-3 times the diameter of the bone [2].
-
Larger osteotomy gaps lead to significantly more fibrocartilage and a lower amount of newly formed blood vessels in the gap healing area compared to osteotomy gaps of medium size.
-
From a clinical point of view, the use of operating techniques that avoid damage to the vascular system and allow reduction of the bone fragments, to achieve small fracture gaps, are important if we are to ensure proper fracture healing.
References
-
Claes et al. Influence of size and stability of the osteotomy gap on the success of fracture healing. J Orthop Res 15, 577-584 (1997).
-
Garcia et al. Rodent animal models of delayed bone healing and non-union formation: a comprehensive review. Eur Cell Matter 26, 1-12 (2013).
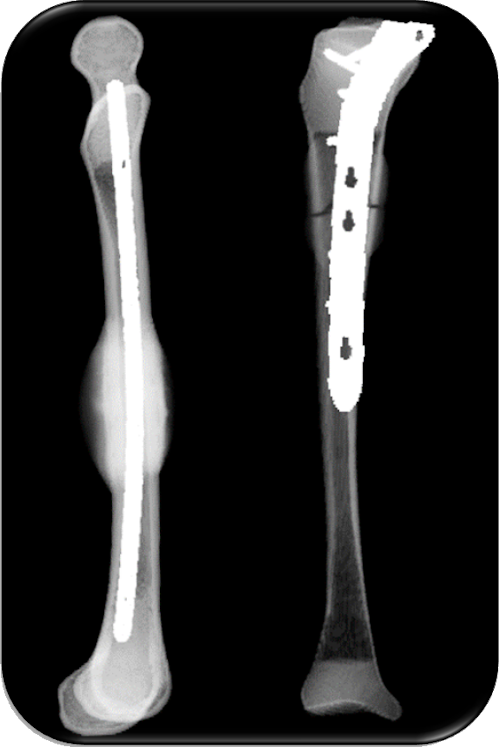
Tibia shaft fractures, different healing pattern of nail and plate

Both nail and and plating systems have become reliable treatment modalities for tibial fractures. [1]
While proponents of each treatment modality will debate on pros and cons of both nailing and plating, there is still no clear consensus on a gold standard.
Stabilization with locking plates can cause inconsistent and asymmetric formation of periosteal callus, which may be attributed to the high stiffness of the fixation construct.
Compared to plate fixation fixation, intramedullary nailing techniques could have short time of union and full weight-bearing, as well as a low risk of infection. [3]
References
Umut Yavuz et al. Comparison of intramedullary nail and plate fixation in
distal tibia diaphyseal fractures close to the mortise. Ulus Travma Acil Cerrahi Derg, Vol. 20 (2014)Weihang Gao et al. Biomechanical comparison of intramedullary nail and plate osteosynthesis for extra-articular proximal tibial fractures with segmental bone defect. Front. Bioeng. Biotechnol., 11, (2023)
Cheng Ren et al. Comparison of intramedullary nailing fixation and percutaneous locked plating fixation for the treatment of proximal tibial fractures: A meta-analysis. Journal of Orthopaedic Surgery. 28(2) (2021)
Advanced concepts
Biomechanics of intramedullary nailing

The intramedullary nail evolved from press-fit fixation to today’s nails that achieve stability through interlocking screws. Important landmarks in the development of nails are the introduction of flexible reaming, the transition from slotted to unslotted nail design, the introduction of “dynamization” of the nail and the use of titanium alloys as a new nail material [1].
- Choosing the largest possible nail diameter makes biomechanical sense due to the superior stiffness it provides [2].
- The play of the nail inside the medullary cavity should be kept as small as possible. Otherwise, the nail would be excessively loose in the cavity, and shear and torsional movements would be produced at the fracture gap.
- Minimizing shear and torsional movements at the gap will promote fracture healing.
- Greater system stiffness, in turn, results in less movement at the fracture gap.
- Suitable fracture patterns like axially stable fractures (e.g. A3) should be meticulously reduced and then compressed.
- Nail dynamization should be performed between three and six months after trauma [3].
References
Umut Yavuz et al. Comparison of intramedullary nail and plate fixation in
distal tibia diaphyseal fractures close to the mortise. Ulus Travma Acil Cerrahi Derg, Vol. 20 (2014)Weihang Gao et al. Biomechanical comparison of intramedullary nail and plate osteosynthesis for extra-articular proximal tibial fractures with segmental bone defect. Front. Bioeng. Biotechnol., 11, (2023)
Cheng Ren et al. Comparison of intramedullary nailing fixation and percutaneous locked plating fixation for the treatment of proximal tibial fractures: A meta-analysis. Journal of Orthopaedic Surgery. 28(2) (2021)
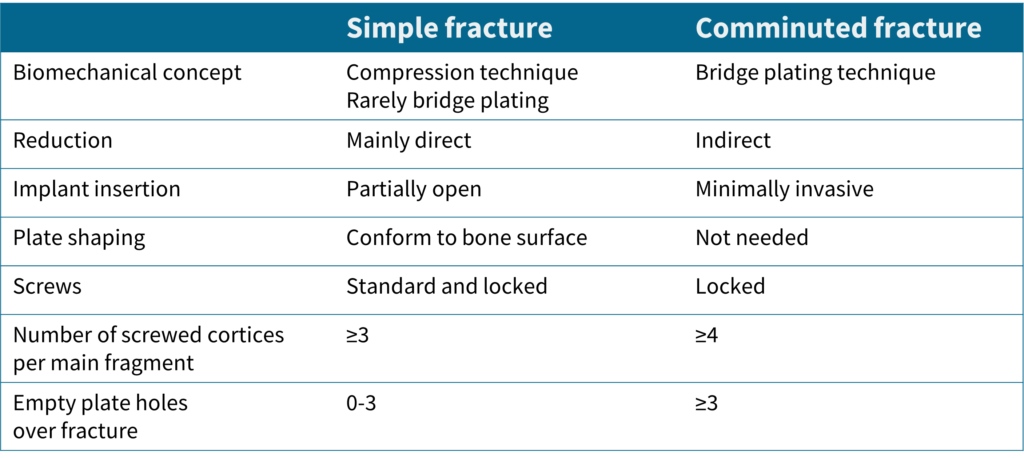
Biomechanics of plate osteosynthesis
Working length:
- The plate working length should be as long as the fracture; if the working length exceeds the fracture length, the fracture will require longer to heal.
- A longer working length only reduces the plate load if the fracture gap closes and the load is shared between the implant and the bone. As healing progresses, the working length also affects the plate stress in the case of a comminuted fracture / fracture with a large gap.
Plate length:
- According to Gautier et al., the length of a plate for a comminuted fracture should be at least 2-3 times the length of the defect [1].
- A longer plate does not harm fracture healing.
Min-Max-Principle:
- Gautier and Sommer recommend holding screws in >3 for simple and >4 cortices for complex fractures [1].
Conclusive rules by Gautier et al.
References
- Emanuel Gautier, Christoph Sommer. Guidelines for the clinical application of the LCP. Injury 34, Supplement 2 (2003).
Intratrochantric fractures
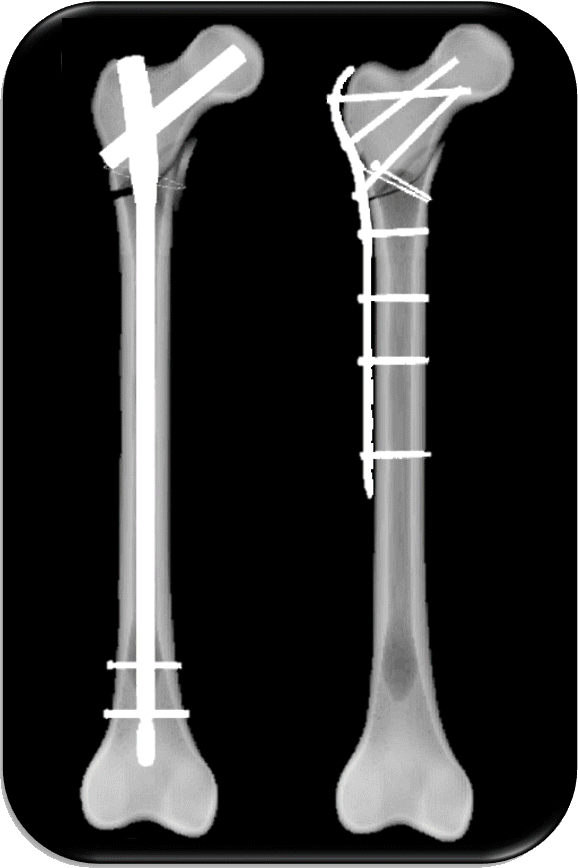
- Subtrochanteric fractures have been treated using intramedullary devices rather than extramedullary implants over the last 25 years [1].
- The treatment of unstable subtrochanteric fracture of the femur with PFNA combined with cerclage wire has the advantages of simple operation, satisfactory reduction of fracture, stable fixation, and good recovery of limb function.
- Due to the long lever arm in the proximal fracture, the nail construct is exposed to a high load.
- LCP plating requires careful attention to biomechanical principles to avoid implant breakage or loosening [2].
References
- Shivashankar et al.. Implantology of Subtrochanteric Fractures. Handbook of Orthopaedic Trauma Implantology 0, 1459–1478 (2023).
- Sommer et al.. Locking compression plate loosening and plate breakage: a report of four cases. J Orthop Trauma 18, 571-577 (2004).